by, Ashley Hodges, PhD, CRNP, WHNP-BC
As a teenager I would hear friends talk about the severity of their menstrual cramps, confident endometriosis was the culprit. I am fairly certain I understood nothing about endometriosis, but soon questioned whether I too was suffering from this disease. It took nursing school for me to realize that I had been blindly following the musings of these young women and likely sounded ridiculous in my own conclusions. It was graduate school and my work as a Woman’s Health Nurse Practitioner where I learned fact from fiction and became well versed in diagnosis and treatment options.
Despite my formal education, it was not until a dear friend; we will call her Lisa, was diagnosed with endometriosis and later labeled infertile that I began to truly see all colors of the disease. My use of the word color is intentional. Read on and you will see why.
What Is Endometriosis?
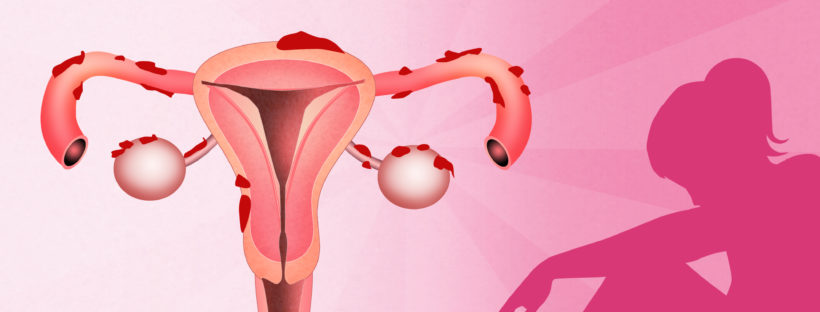
Endometriosis is a chronic disease of estrogen-dependent lesions of endometrial glands and stroma found outside the uterus (Rogers, 2013). Endometriosis is most commonly found on the ovaries, the fallopian tubes, the bowel, and the areas in front, in back, and to the sides of the uterus. Endometriosis affects approximately 5 million women in the United States. (American College of Obstetricians and Gynecologists , 2010). However, the actual numbers are unknown since endometriosis is often goes undiagnosed due to lack of symptoms and difficulty or delay in diagnosis.
Misconceptions about Endometriosis
- Endometriosis is fast and easy to diagnose.
FALSE. It has been estimated that the time between the onset of symptoms and surgical diagnosis of endometriosis is 6.7 years.
- Endometriosis is always painful.
FALSE. Not all patients with endometriosis experience pain. When women do experience pain, timing may be before, during, or between periods. Some women experience pain during or after intercourse. Others may experience pain with bowel movements, especially during the menstrual cycle.
- Hormonal treatments cure endometriosis.
FALSE.. There is no cure for endometriosis. Hormonal suppressive therapy does improve pain symptoms. However, recurrence rates are high after the medication is discontinued (American College of Obstetricians and Gynecologists, 2010).
- Women with endometriosis are infertile.
FALSE. This is not necessarily the case although up to 50% of women with endometriosis have difficulty conceiving naturally (American Society for Reproductive Medicine, 2012).
Lisa’s Story
At the age of 24 Lisa knew something was not right. Being a nurse she could only justify so much about her heavy, frequent and painful periods. Sex was painful, but maybe it was her state of mind or the bad relationship. She had moved to a new town only 2 years before, far from her less- than- thrilled parents. She was working long hard hours in the Neuro ICU and had little time for a social life. Lisa and Brian had been dating for over a year and his anger over her long hours and lack of attention to intimacy was worsening. This, she thought, was why her health was so poor. Today, 22 years later, Lisa admits she knew something else was wrong, but denial was the easiest path at the time.
By the age of 28, Lisa’s symptoms were worsening, missed days from work putting her job at risk. She and Brian married that year. Her symptoms worsened over the next year with sex becoming unbearable. One afternoon at work she noticed blood in her stool following a painful bowel movement, but wrote it off to hemorrhoids, being on her feet all day as a nurse. That evening Lisa spoke to her mother, listing off her most recent symptoms of back and leg pain, abdominal pain, and nausea. Lisa decided it was time to see her provider and discuss her recent and recurrent symptoms. That night. Lisa woke in the middle of the night with severe lower abdominal pain which led her to seek care in the emergency department.
Lisa was taken to the OR and a right ovarian cyst the size of a softball was removed. Upon waking from surgery, Lisa was told of the ovarian cyst diagnosis. It was not until the next morning she was informed of the other findings. Lisa had severe endometriosis on her uterus, fallopian tubes, ovaries, ureters, bowel and bladder.
Lisa was told the chance of her conceiving naturally was likely nonexistent and that assisted reproduction was the only hope. Lisa underwent surgery to remove large areas of endometrial lesions and received six months of Leuprolide. She tried to conceive without any other medical intervention for three months without success. Fearful of worsening endometriosis she elected to take three months of ovulation induction medication, again without success. Lisa was given the option of moving forward with other reproductive assistance, but due to the cost, elected to wait and save money. Unfortunately, Lisa was back in the OR just six months later for additional surgery including a hysterectomy.
Today Lisa continues to struggle with complications from scarring and recurrent endometrial lesion implants. Lisa and Brian elected to adopt a child who is now 2 years old and are hoping to adopt again soon. Unfortunately Lisa’s story is not unique. More options are available for women today in the treatment of endometriosis but the struggle continues.
What is the reason behind the word “color” in this post’s title? Lisa saw many providers and sought support and guidance through more nontraditional methods. At one visit to an alternative methods provider, she was told to give a color to the endometriosis and then to not own anything of that color. She later told me that she gave endometriosis the color brown… because endometriosis was one big (beep).
Learn more about this topic at: http://endometriosisfoundation.org/
 Dr. Ashley Hodges is an Associate Professor and Assistant Dean for Graduate Clinical Programs at the University of Alabama at Birmingham School of Nursing. She is certified as a Women’s Health Nurse Practitioner and has over 25 years of experience in maternal child nursing, administration and nursing education. She was recently named in the Top 20 Outstanding Professors of Women’s Health Nursing by Nurse Practitioner Schools. Dr. Hodges served a two-year term as Board Member for AWHONN beginning in 2014 and was the 2015 Chair of the Public Policy Committee. She is currently a member of the editorial advisory board for the journal Nursing for Women’s Health.
Dr. Ashley Hodges is an Associate Professor and Assistant Dean for Graduate Clinical Programs at the University of Alabama at Birmingham School of Nursing. She is certified as a Women’s Health Nurse Practitioner and has over 25 years of experience in maternal child nursing, administration and nursing education. She was recently named in the Top 20 Outstanding Professors of Women’s Health Nursing by Nurse Practitioner Schools. Dr. Hodges served a two-year term as Board Member for AWHONN beginning in 2014 and was the 2015 Chair of the Public Policy Committee. She is currently a member of the editorial advisory board for the journal Nursing for Women’s Health.
RESOURCES
American College of Obstetricians and Gynecologists. (2010). Management of endometriosis (Practice Bulletin No. 114). Obstetrics & Gynecology, 116(1), 223-236
American Society for Reproductive Medicine. (2012). Endometriosis and infertility: a committee opinion. Fertility and Sterility, 98, 591-598.
Rogers, P. A., D’Hooghe, T. M., Fazleabas, A., Giudice, L. C., Montgomery, G. W., Petraglia, F., & Taylor, R. N. (2013) Defining future directions for endometriosis research. Reproductive Sciences, 20(5), 483-499.